Sarampión y comportamiento del sistema inmunológico
Sarampión y respuesta inmune
DOI:
https://doi.org/10.47993/gmb.v48i2.1121Palabras clave:
inmunosupresión, memoria inmunológica, respuesta inmune, virus del sarampiónResumen
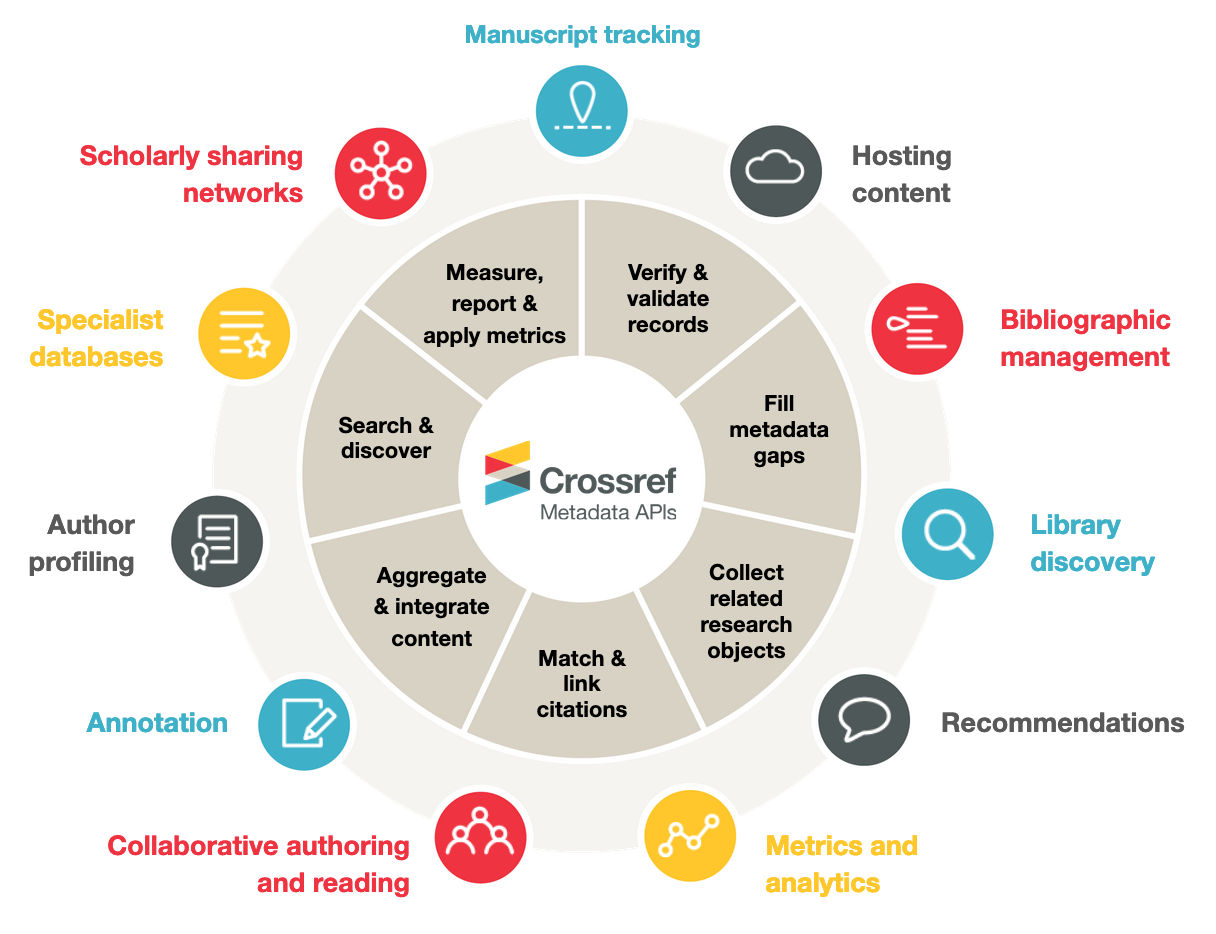
Introducción: Este artículo revisa el comportamiento del sistema inmunológico frente al virus del sarampión (MeV), Objetivo: Describir los mecanismos de la respuesta inmune desencadenada por MeV. Métodos: Se realizó una revisión sistemática de literatura científica, incluyendo estudios inmunológicos y clínicos publicados en PubMed, Scopus y Web of Science, utilizando términos MeSH/DeCS como MeV, y respuesta inmunológica. Desarrollo: El MeV, sea mediante infección natural o por vacunación, activa a la respuesta inmunológica pero también genera efectos inmunosupresores e inmunoamnesia. Se destaca la acción de los mecanismos innatos: interferones, células NK y adaptativos: linfocitos T CD8+/CD4+ y producción de anticuerpos neutralizantes; la inducción de inmunosupresión mediante apoptosis de linfocitos de memoria, reduciendo la protección contra otras infecciones. Conclusión: La vacunación con cepas atenuadas genera inmunidad robusta, evitando los efectos de inmunosupresión e inmunoamnesia, por lo que se destaca la importancia de mantener altas coberturas vacunales para prevenir la enfermedad y sus complicaciones.
Métricas
Citas
Moss WJ. Measles. Lancet. 2017;390(10111):2490-2502. doi: 10.1016/S0140-6736(17)31463-0. DOI: https://doi.org/10.1016/S0140-6736(17)31463-0
Rota PA, Moss WJ, Takeda M, de Swart RL, Thompson KM, Goodson JL. Measles. Nat Rev Dis Primers. 2016;2:16049. doi: 10.1038/nrdp.2016.49. DOI: https://doi.org/10.1038/nrdp.2016.49
Gadroen K, Dodd CN, Masclee GMC, van de Garde EMW, van der Woude CJ, Stehouwer CDA, et al. Impact and longevity of measles-associated immune suppression: a matched cohort study using data from the THIN general practice database in the UK. BMJ Open. 2018;8(4):e021465. doi: 10.1136/bmjopen-2017-021465. DOI: https://doi.org/10.1136/bmjopen-2017-021465
Daruna J. Immune system basics. In: Daruna JH, editor. Introduction to psychoneuroimmunology. 2nd ed. San Diego: Academic Press; 2012. p. 27-61. doi: 10.1016/B978-0-12-382049-5.00003-6. DOI: https://doi.org/10.1016/B978-0-12-382049-5.00003-6
Medina KL. Overview of the immune system. Handb Clin Neurol. 2016;133:61-76. doi: 10.1016/B978-0-444-63432-0.00004-9. DOI: https://doi.org/10.1016/B978-0-444-63432-0.00004-9
World Health Organization. Global eradication of measles: report by the secretariat [Internet]. Geneva: WHO; 2010 [citado 2025 Dec 17]. Disponible en: https://apps.who.int/gb/ebwha/pdf_files/wha63/a63_18-en.pdf.
Guerra FM, Crowcroft NS, Friedman L, Maclsaac K, Howe N, Halperin SA, et al. Waning of measles maternal antibody in infants in measles elimination settings - a systematic literature review. Vaccine. 2018;36(8):1248-55. doi: 10.1016/j.vaccine.2018.01.002. DOI: https://doi.org/10.1016/j.vaccine.2018.01.002
Schenk J, Abrams S, Theeten H, Van Damme P, Beutels P, Hens N. Immunogenicity and persistence of trivalent measles, mumps, and rubella vaccines: a systematic review and meta-analysis. Lancet Infect Dis. 2021;21(2):286-95. doi: 10.1016/S1473-3099(20)30442-4. DOI: https://doi.org/10.1016/S1473-3099(20)30442-4
Takeda M, Tahara M, Nagata N, Seki F. Wild-type measles virus is intrinsically dual-tropic. Front Microbiol. 2012;2:279. doi: 10.3389/fmicb.2011.00279. DOI: https://doi.org/10.3389/fmicb.2011.00279
Amurri L, Reynard O, Gerlier D, Horvat B, Iampietro M. Measles virus-induced host immunity and mechanisms of viral evasion. Viruses. 2022;14(12):2641. doi: 10.3390/v14122641. DOI: https://doi.org/10.3390/v14122641
Vizzotti C, Harris JB, Aquino A, Bruni L, Bonino F, Canil L, et al. Immune response to co-administration of measles, mumps, and rubella (MMR), and yellow fever vaccines: a randomized non-inferiority trial among one-year-old children in Argentina. BMC Infect Dis. 2023;23:165. doi: 10.1186/s12879-023-08114-1. DOI: https://doi.org/10.1186/s12879-023-08114-1
Ferreira CSM, Perin MCAA, Moraes-Pinto MI, Simão-Gurge RM, Goulart AL, Weckx LY, et al. Humoral immune response to measles and varicella vaccination in former very low birth weight preterm infants. Braz J Infect Dis. 2018;22(1):41-6. doi: 10.1016/j.bjid.2017.12.001. DOI: https://doi.org/10.1016/j.bjid.2017.12.001
Do LAH, Mulholland K. Measles 2025. N Engl J Med. 2025. doi: 10.1056/NEJMra2504516. DOI: https://doi.org/10.1056/NEJMra2504516
Schneider-Schaulies S, ter Meulen V. Modulation of immune functions by measles virus. Springer Semin Immunopathol. 2002;24(2):127-48. doi: 10.1007/s00281-002-0101-3. DOI: https://doi.org/10.1007/s00281-002-0101-3
Griffin DE. Measles virus-induced suppression of immune responses. Immunol Rev. 2010;236:176-89. doi: 10.1111/j.1600-065X.2010.00925.x. DOI: https://doi.org/10.1111/j.1600-065X.2010.00925.x
van Binnendijk RS, Poelen MCM, Kuijpers KC, Osterhaus ADME, Uytdehaag FGC. The predominance of CD8+ T cells after infection with measles virus suggests a role for CD8+ class I MHC-restricted cytotoxic T lymphocytes (CTL) in recovery from measles. J Immunol. 1990;144(6):2394-9. DOI: https://doi.org/10.4049/jimmunol.144.6.2394
Permar SR, Griffin DE, Letvin NL. Immune containment and consequences of measles virus infection in healthy and immunocompromised individuals. Clin Vaccine Immunol. 2006;13(4):437-43. doi: 10.1128/CVI.13.4.437-443.2006. DOI: https://doi.org/10.1128/CVI.13.4.437-443.2006
Griffin DE, Ward BJ, Jauregui E, Johnson RT, Vaisberg A. Immune activation during measles: interferon-gamma and neopterin in plasma and cerebrospinal fluid in complicated and uncomplicated disease. J Infect Dis. 1990;161(3):449-53. doi: 10.1093/infdis/161.3.449. DOI: https://doi.org/10.1093/infdis/161.3.449
Griffin DE, Ward BJ, Jauregui E, Johnson RT, Vaisberg A. Immune activation in measles. N Engl J Med. 1989;320(25):1667-72. doi: 10.1056/NEJM198906223202506. DOI: https://doi.org/10.1056/NEJM198906223202506
Akdis M, Burgler S, Crameri R, Eiwegger T, Fujita H, Gomez E, et al. Interleukins, from 1 to 37, and interferon-γ: receptors, functions, and roles in diseases. J Allergy Clin Immunol. 2011;127(3):701-21.e1-70. doi: 10.1016/j.jaci.2010.11.050. DOI: https://doi.org/10.1016/j.jaci.2010.11.050
Naniche D. Human immunology of measles virus infection. In: Griffin DE, Oldstone MBA, editors. Measles. Berlin: Springer; 2009. p. 151-71. doi: 10.1007/978-3-540-70617-5_8. DOI: https://doi.org/10.1007/978-3-540-70617-5_8
Helfand RF, Kebede S, Gary HE Jr, Beyene H, Bellini WJ. Timing of development of measles-specific immunoglobulin M and G after primary measles vaccination. Clin Diagn Lab Immunol. 1999;6(2):178-80. doi: 10.1128/CDLI.6.2.178-180.1999. DOI: https://doi.org/10.1128/CDLI.6.2.178-180.1999
Nic Lochlainn LM, de Gier B, van der Maas N, Hahné S, de Melker H, Knol M. Effect of measles vaccination in infants younger than 9 months on the immune response to subsequent measles vaccine doses: a systematic review and meta-analysis. Lancet Infect Dis. 2019;19(11):1246-54. doi: 10.1016/S1473-3099(19)30396-2. DOI: https://doi.org/10.1016/S1473-3099(19)30396-2
Griffin DE. Measles immunity and immunosuppression. Curr Opin Virol. 2021;46:9-14. doi: 10.1016/j.coviro.2020.08.002. DOI: https://doi.org/10.1016/j.coviro.2020.08.002
Tranter I, Smoll N, Lau CL, Rocklöv J, Quilty BJ, Clifford S, et al. Onward virus transmission after measles secondary vaccination failure. Emerg Infect Dis. 2024;30(9):1747-54. doi: 10.3201/eid3009.240150. DOI: https://doi.org/10.3201/eid3009.240150
Iwasa T, Suga S, Qi L, Komada Y. Apoptosis of human peripheral blood mononuclear cells by wild-type measles virus infection is induced by interaction of hemagglutinin protein and cellular receptor, SLAM via caspase-dependent pathway. Microbiol Immunol. 2010;54(7):405-16. doi: 10.1111/j.1348-0421.2010.00231.x. DOI: https://doi.org/10.1111/j.1348-0421.2010.00231.x
de Vries RD, McQuaid S, van Amerongen G, Yuksel S, Verheyen AT, Osterhaus AD, et al. Measles immune suppression: lessons from the macaque model. PLoS Pathog. 2012;8(8):e1002885. doi: 10.1371/journal.ppat.1002885. DOI: https://doi.org/10.1371/journal.ppat.1002885
Morales GB, Muñoz MA. Immune amnesia induced by measles and its effects on concurrent epidemics. J R Soc Interface. 2021;18(179):20210153. doi: 10.1098/rsif.2021.0153. DOI: https://doi.org/10.1098/rsif.2021.0153
Laksono BM, de Vries RD, Verburgh RJ, Visser EG, de Jong A, Fraaij PLA, et al. Studies into the mechanism of measles-associated immune suppression during a measles outbreak in the Netherlands. Nat Commun. 2018;9(1):4944. doi: 10.1038/s41467-018-07515-0. DOI: https://doi.org/10.1038/s41467-018-07515-0
Haeryfar SMM. On invariant T cells and measles: a theory of "innate immune amnesia". PLoS Pathog. 2020;16(12):e1009071. doi: 10.1371/journal.ppat.1009071. DOI: https://doi.org/10.1371/journal.ppat.1009071
Albarbar BS. Human immune responses to measles virus: a literature review. J Microbiol Infect Dis. 2024;14(3):103-8. doi: 10.5455/JMID.2024.v14.i3.3. DOI: https://doi.org/10.5455/JMID.2024.v14.i3.3
Oglesbee MJ, Pratt M, Carsillo T. Role for heat shock proteins in the immune response to measles virus infection. Viral Immunol. 2002;15(3):399-416. doi: 10.1089/088282402760312296. DOI: https://doi.org/10.1089/088282402760312296
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2025 Gaceta Médica Boliviana

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial 4.0.