Covid-19, una mirada desde la pediatría
Palabras clave:
coronavirus, Covid-19, pediatría, pandemia, SARS-CoV-2Resumen
El COVID-19 fue predominantemente más prevalente entre adultos mayores de 15 años en las primeras etapas del brote y la proporción de casos confirmados entre niños fue relativamente menor. Sin embargo, debido a la creciente propagación mundial del SARS-CoV-2, tenemos nuevos desafíos para la prevención y el control de la epidemia de COVID-19 entre los niños. Ya que en los más pequeños no se pueden emplear medidas de prevención (barbijos), la clínica inespecífica que presentan, las dificultades para el diagnóstico, la deficiente comunicación entre médico-paciente y familiar que han contribuido al desafío de desarrollar medidas para proteger a esta población, al igual que al personal de salud que manejan casos pediátricos. Al mismo tiempo, los niños con comorbilidades, s on vulnerables a la infección por SARS-CoV-2. La presente revisión intenta mostrar esta enfermedad desde el punto de vista pediátrico, para orientar en su diagnóstico y manejo.
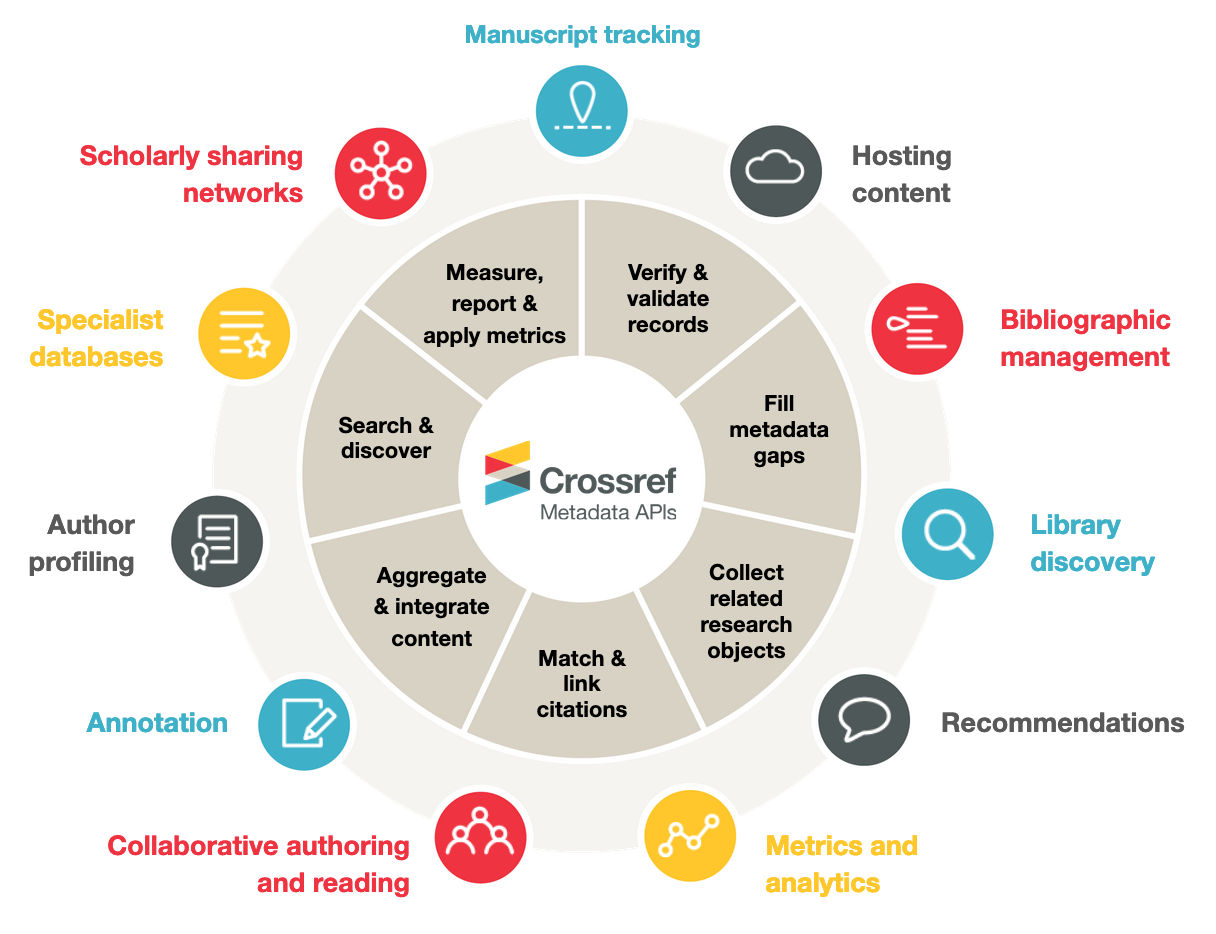
Métricas
Citas
Calvo C, et al. Recomendaciones sobre el manejo clínico de la infección por el «nuevo coronavirus» SARS-CoV2. Grupo de trabajo de la Asociación Española de Pediatría (AEP). An Pediatr (Barc). 2020. https://doi.org/10.1016/j.anpedi.2020.02.001. [ Links ]
She Jiatong, Liu Wenjun. Epidemiological characteristics and prevention and control measures of Corona Virus Disease 2019 in children. Journal of Tropical Medicine, 2020. [ Links ]ISSN 1672-3619, CN 44-1503/R. http://kns.cnki.net/kcms/detail/44.1503.R.20200217.1638.002.html.
She Jiatong, Liu Lanqin, Liu Wenjun. COVID-19 epidemic: disease characteristics in children. Journal of Medical Virology, 2020. [ Links ] https://doi:10.1002/jmv.25807.
World Health Organization.WHO characterizes COVID-19 as a pandemic. 1.1 [EB/OL] (2020-03-12) [2020-03-12]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen.
Matthew C. Wong, Sara J. Javornik Cregeen, Nadim J. Ajami, et al. Evidence of recombination in coronaviruses implicating pangolin origins of 2019-nCoV [J]. BioRxiv, 2020. DOI: https://doi.org/10.1101/2020.02.07.939207.
Qiang Zhou, Renhong Yan, Yuanyuan Zhang, et al. Structure of dimeric full-length human ACE2 in complex with B0ATI [J]. BioRxiv, 2020. DOI: https://doi.org/10.1101/2020.02.17.951848.
Tran Thi, Nhu Thao, Fabien Labroussaa, Nadine Ebert, et al. Rapid reconstruction of SARS-CoV-2 using a synthetic genomics platform [J]. Bio Rxiv, 2020. DOI: https://doi.org/10.1101/2020.02.21.959817.
Xiaolu Tang, Changcheng Wu, Xiang Li, et al. On the origin and continuing evolution of SARS-CoV-2 [J]. National Science Review, nwaa036. https://doi.org/10.1093/nsr/nwaa036.
Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020; 395(10223): 514-523. [ Links ] Doi: 10.1016/S0140-6736(20)30154-9. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30154-9/fulltext.
Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020. [ Links ] doi: 10.1056/NEJMoa2002032.
Xing Y-H, Ni W, Wu Q, Li W-J, Li G-J, Wang W-D, Tong J-N, Song X-F, Wing-Kin, Wong G, Xing Q-S, Prolonged Viral Shedding in Feces of Pediatric Patients with Coronavirus Disease 2019, Journal of Microbiology, Immunology and Infection, https://doi.org/10.1016/j.jmii.2020.03.021.
Yang Lifen, Dai Zhenyuan, Duan Mengqi, et al. Suggestions for medical staff from department of pediatrics during the treatment of 2019-nCoV infection/pneumonia [J]. Journal of New Medicine, 2020. ISSN 0253-9802, CN 44-1211/R. https://DOI:10.3969/j.ISSN 0253-9802.2020.02.001.
Dong Y, Mo X, Hu Y, et al. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics. 2020. [ Links ] https://doi: 10.1542/peds.2020-0702. https://pediatrics.aappublications.org/content/early/2020/03/16/peds.2020-0702.1/tab-article-info
Fang F, Zhao D, Chen Y, et al. Recommendations for the diagnosis, prevention and control of the 2019 novel coronavirus infection in children (first interim edition) [Chinese]. Chinese Journal of Pediatrics. In press.
Centers for Disease Control and Prevention. Interim Clinical Guidance for Management of Patients with Confirmed 2019 Novel Coronavirus (2019-nCoV) Infection, Updated February 12, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html (Accessed on February 14, 2020). [ Links ]
World Health Organization. Novel Coronavirus (2019-nCoV) technical guidance: Patient management. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/patient-management (Accessed on February 02, 2020). [ Links ]
Delaney JW, Pinto R, Long J, Lamontagne F, Adhikari NK, Kumar A, et al. The influence of corticosteroid treatment on the outcome of influenza A (H1N1pdm09)-related critical illness. Crit Care. 2016; 20:75.
https://dgsurgent.sante.gouv.fr/dgsurgent/ inter/details Message Builder.do?id=30500&cmd=visualizer Message (Accessed on March 19, 2020). [ Links ]
Day M. Covid-19: ibuprofen should not be used for managing symptoms, say doctors and scientists. BMJ 2020; 368:m1086.
Updated: WHO Now Doesn’t Recommend Avoiding Ibuprofen For COVID-19 Symptoms. Science Alert 2020. [ Links ]
https://www.sciencealert.com/who-recommends-to-avoid-taking-ibuprofen-for-covid-19-symptoms (Accessed on March 19, 2020).
Ray WA, Murray KT, Hall K, Arbogast PG, Stein CM. Azithromycin and the risk of cardiovascular death. N Engl J Med. 2012 May 17; 366(20):1881-90. [ Links ] doi: 10.1056/NEJMoa1003833.
Appel GB, Neu HC. The nephrotoxicity of antimicrobial agents (second of three parts). N Engl J Med. 1977 Mar 31; 296(13):722-8. [ Links ]
Yao X, Ye F, Zhang M, Cui C, Huang B, Niu P, Liu X, Zhao L, Dong E, Song C, Zhan S, Lu R, Li H, Tan W, Liu D. In Vitro Antiviral Activity and Projection of Optimized Dosing Design of Hydroxychloroquine for the Treatment of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Clin Infect Dis. 2020. [ Links ]
Chen Z, Hu J, Zhang Z, et al. Efficacy of hydrochlroquine in patients with COVID-19: Results of a randomized trial. Unpublished. https://www.medrxiv.org/content/10.1101/2020.03.22.20040758v2 (Accessed on April 01, 2020).
Gautret et al. Hydroxychloroquine and azithromycin as a treatment of COVID‐19: results of an open‐label non‐randomized clinical trial. International Journal of Antimicrobial Agents – In Press 17 March 2020 DOI:10.1016/j.ijantimicag.2020.105949.
Chen J, Lui D, Lui L, et al. A pilot study of hydroxychloroquine in treatment of patients with common coronavirus disease-19 (COVID-19). Journal of Zhejiang University 2020.
Gao J, Tian Z, and Yang X. Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Biosci Trends 2020; 14:72.
US Food and Drug Administration. https://www.fda.gov/media/136534/download [ Links ] (Accessed on March 30, 2020).
Sheahan TP, Sims AC, Graham RL, et al. Broad-spectrum antiviral GS-5734 inhibits both epidemic and zoonotic coronaviruses. Sci Transl Med 2017; 9.
Wang M, Cao R, Zhang L, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res 2020; 30:269. [ Links ]
Cai Q, Yang M, Liu D, et al. Experimental Treatment with Favipiravir for COVID-19: An Open-Label Control Study. Engineering 2020.
Groneberg DA, Poutanen SM, Low DE, et al. Treatment and vaccines for severe acute respiratory syndrome. Lancet Infect Dis 2005; 5:147. [ Links ]
Cao B, Wang Y, Wen D, et al. A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19. N Engl J Med 2020.
National Health Commission of People’s Republic of China. Diagnosis and treatment of pneumonia caused by novel corona- virus (trial versión 4). 2020. https://www.nhc.gov.cn/xcs/zhengcwj/202001/4294563ed35b43209b31739bd0785e67/files/7a930 9111267475a99d4306962c8bf78.pdf . [ Links ]
S. Bialek, R. Gierke, M. Hughes, L. McNamara, T. Pilishvilli and T. Skoff. Coronavirus Disease 2019 in Children. United States, February 12–April 2, 2020, Prevention Morbidity and Mortality Weekly Report, pp. 1-5, 2020.
S. Jaqueline, M. BChir, A. Tosoni, K. YaeJean, K. Niranjan and M. Srinivas. Coronavirus Disease 2019 in Critically Ill. Pediatric Critical Care Medicine, pp. 1-5, 2020.
SECIP, Documento de manejo clínico del paciente pediátrico con infección por SAR-CoV-2 en cuidados intensivos. Sociedad Española de Cuidados Intensivos Pediátricos, pp. 1-19, 2020.
Sociedad Peruana de Medicina Intensiva. Documento de consenso para el manejo del niño crítico con COVID-19. Capítulo de Medicina Intensiva Pediátrica, pp. 1-27, 2020. [ Links ]
T. Cook, K. El-Boghdadly, B. McGuire, A. McNarry, A. Patel and A. Higgs. Consensus guidelines for managing the airway in patients with COVID-19. Anaesthesia, pp. 1-15, 2020.
E. Núñez. Y. Herrán. P. Serrudo. J. Potosí, H. Ramírez. H. Suárez and D. Peñarrieta, Guía de manejo en el abordaje clínico del paciente pediátrico con infección por COVID-19 para Unidades de Terapia Intensiva Pediátrica. Sociedad Boliviana de Terapia Intensiva Pediátrica, pp. 1-14, 2020.
W. Alhazzani. M. Hylander. Y. Arabi. M. Loeb. M. Ng Gong. E. Fan and Oczkowski. Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill Adults with Coronavirus Disease 2019 (COVID-19). Critical Care Medicine, 2020.
M. Kneyber, A. Medina, V. Alapont , R. Blokpoel, J. Brierley, G. Chidini and M. Garcia, Practice recommendations for the management of children with suspected or proven COVID-19 infections from the PEMVECC and the section Respiratory Failure from the ESPNIC. European Society for Paediatric and Neonatal Intensive Care, pp. 1-7, 2020.
R. Adasme. D. Wood. F. Bustos. I. Sepúlveda and P. Figueroa. Guía de Recomendaciones de Armado y Uso de Filtros en Ventilación Mecánica COVID19. Sociedad Chilena de Medicina Intensiva, pp. 1-33, 2020.
SPMCYCI, Recomendaciones manejo COVID-19 en Terapia Intensiva – SPMCYCI. Sociedad Paraguaya de Medicina Crítica y Cuidados Intensivos, 2020. [ Links ]
D. Edelson. C. Sasson. P. Chan, D. Atkins. K. Aziz. L. Becker and R. Berg. Interim Guidance for Life Support for COVID-19. 2020. Circulation AHA, pp. 1-18.
Resuscitation Council UK. Guidance on the resuscitation of paediatric patients with suspected or confirmed COVID-19, Resuscitation Council UK, 2020. [ Links ]
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2020 Gaceta Medica Boliviana

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.