Invisibility, the Perspective of the Elderly in a Southeastern Mexican State
DOI:
https://doi.org/10.47993/gmb.v44i2.290Keywords:
Older adult, abuse, invisibility, qualitative researchAbstract
Objective: to analyze the perspectives of the elderly about the conditions that intervene in invisibility. Methods: qualitative research based on fundamental theory was carried out in older adults. To obtain the perspectives on invisibility, we worked under an inductive approach with two focus groups, an interview guide was used with triggering questions in which the categories related to the focus on old age and the family, health care and environment and the society. For the analysis of qualitative data, MAXQDA version 2018.2 software was used. Results: invisibility in the elderly was presented in the family and in society through abandonment, verbal abuse based on insults, humiliation, lack of respect, scolding and teasing, leading to physical aggression. This phenomenon was also observed in health care when they do not listen carefully, do not provide their medications and make them wait a long time to be treated. The emotional effects caused by the invisibility that they express are feeling ignored, forgotten and angry to the point of crying and sadness. Conclusions: the perspectives of older adults allow us to conclude that abuse is one of the manifestations of invisibility that they suffer in three aspects of their lives: the family nucleus, society and healthcare. Invisibility is a challenge and a priority for social and health institutions, since it produces a psychological and moral wound that must be detected in a timely manner.
Metrics
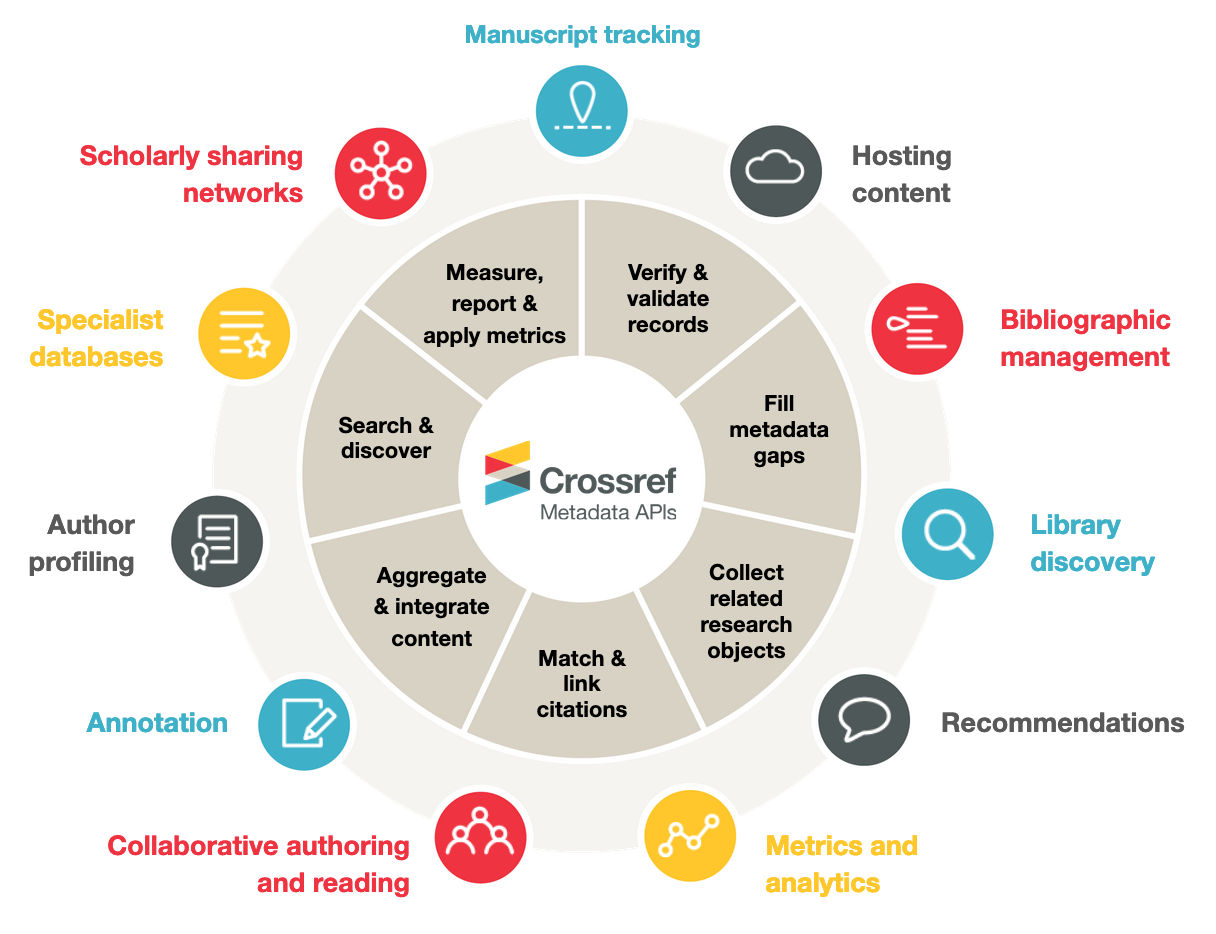
References
Bourdin JC. La invisibilidad social Como violencia. universitas philosophica. 2010; 15-33.
Weisheimer N. La invisibilidad social de las juventudes rurales. Rev. Desidades. 2013; 1(1).
Setel PW, Macfarlane S.B, Szreter S, Mikkelsen L, Jha P, Stout S, AbouZahr C. A scandal of invisibility: making everyone count by counting everyone, The Lancet. 2007; 370 (9598): 1569-1577. https://doi.org/10.1016/S0140-6736(07)61307-5 DOI: https://doi.org/10.1016/S0140-6736(07)61307-5
Sesko Ak, Biernat M. Prototypes of race and gender: The invisibility of Black women, Journal of Experimental Social Psychology. 2010; 46(2): 356-360. DOI: doi.org/10.1016/j.jesp.2009.10.016. https://www.sciencedirect.com/science/article/pii/S0022103109002698 DOI: https://doi.org/10.1016/j.jesp.2009.10.016
Franklin, AJ y Boyd-Franklin, N. Síndrome de invisibilidad: un modelo clínico de los efectos del racismo en los hombres afroamericanos. American Journal of Orthopsychiatry. 2000: 70 (1); 33-41. https://doi.org/10.1037/h0087691 Invisibility syndrome: A clinical model of the effects of racism on African-American males. DOI: https://doi.org/10.1037/h0087691
Eke O, Otugo O, Isom J. Black women in medicine-rising above invisibility. The Lancet. Perspectives the art of medicine. 2021; 397: 573-574. DOI: https://doi.org/10.1016/S0140-6736(21)00302-0 DOI: https://doi.org/10.1016/S0140-6736(21)00302-0
Farley m. Prostitution and the invisibility of harm. Women Terapy. 2003; 3-4: 247-280. https://doi.org/10.1300/J015v26n03_06 DOI: https://doi.org/10.1300/J015v26n03_06
Curtice K, Choo E. Indigenous populations: left behind in the COVID-19 response. The Penumbra see Comment Lancet. 2019; 394: 453 and Perspectives. Lancet. 2020; 395: 1333. DOI: https://doi.org/10.1016/S0140-6736(20)31242-3 DOI: https://doi.org/10.1016/S0140-6736(20)31242-3
Horton R. The continuing invisibility of women and children. The Lancet. 2010;375(9730):1941-1943. DOI: https://doi.org/10.1016/S0140-6736(10)60902-6
The weight of invisibility. The Lancet Global Health.2019. VOLUME 7, ISSUE 7, E808. 2019;. DOI: https://doi.org/10.1016/S2214-109X(19)30219-0 DOI: https://doi.org/10.1016/S2214-109X(19)30219-0
Bourdin JC. La invisibilidad social Como violencia. universitas philosophica. 2010; 54: 15-33.
Buitrago F, Ciurana R, Fernández MC,Tizón JL, Pandemia de la COVID-19 y salud mental: reflexiones iniciales desde la atención primaria de salud española, REv. Atención Primaria. 2021; 53 1: 89-101, https://doi.org/10.1016/j.aprim.2020.06.006. En https://www.sciencedirect.com/science/article/pii/S0212656720301876 DOI: https://doi.org/10.1016/j.aprim.2020.06.006
Poches, D., Meza, J. Maltrato en la población adulta mayor: una revisión. Espacio Abierto. 2017; 26(2): 245-26.
Agudelo M.C., Cardona, D., Segura, A., Muñoz, A., Restrepo, D. Características sociales y familiares asociadas al maltrato al adulto mayor de Pasto, Colombia 2016. Rev CES Psico. 2019; 12(1): 32-42. DOI: https://doi.org/10.21615/cesp.12.1.3
Carnota-Lauzán Orlando. La invisibilidad del paciente: una alarma en la prestación de servicios de salud. Horiz. sanitario. 2020; 19(1): 7-8. Disponible en: http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S200774592020000100007&lng=es DOI: https://doi.org/10.19136/hs.a19n1.3622
Yon Y, Mikton CR, Gassoumis ZD, Wilber KH. Elder abuse prevalence in community settings: a systematic review and meta-analysis. Lancet Glob Health. 2017; 5: 47-56. DOI: https://doi.org/10.1016/S2214-109X(17)30006-2
OMS. Comunicado de Prensa. Ginebra: OMS; 2017. Disponible en: http://www.who.int/mediacentre/news/releases/2017/abuse-older-people/es/
Glaser, Barney y Strauss, Anselm. (1967). The Discovery of Grounded Theory. Chicago, Aldine.
Burnes D, Lachs M, Burnette D, Pillemer K, Variables evaluaciones del maltrato de ancianos entre víctimas: Hallazgos de un estudio basado en la población, The Journals of Gerontology: Serie B. 2019; 74(5): 881-890. https://doi.org/10.1093/geronb/gbx005 DOI: https://doi.org/10.1093/geronb/gbx005
Vinueza MF, Núñez Y, Leyva MA, Montero IL, Mera CM. Determinantes sociodemográficos de violencia en adultos mayores ecuatorianos, Revista Española de Geriatría y Gerontología. 2021; 56(1): 41-46. https://doi.org/10.1016/j.regg.2020.06.003 DOI: https://doi.org/10.1016/j.regg.2020.06.003
Pabón Poches, Daysy Katherine, Delgado Meza, Jesús Armando, Maltrato en la población adulta mayor: una revisión. Espacio Abierto. 2017; 26 (2): 245-267. Disponible en: https://www.redalyc.org/articulo.oa?id=12252818014
Cohen J, Hazan H, Lerman Y, Shalom V. Correlates and predictors of loneliness in older-adults: a review of quantitative results informed by qualitative insights. Int Psychogeriatr. 2016; 28(4):557- 76. doi: 10.1017/S1041610215001532. PMID: 26424033. DOI: https://doi.org/10.1017/S1041610215001532
Chang E, Levy BR. High Prevalence of Elder Abuse During the COVID-19 Pandemic: Risk and Resilience Factors. The American Journal of Geriatric Psychiatry, 2021. https://doi.org/10.1016/j.jagp.2021.01.007 DOI: https://doi.org/10.1016/j.jagp.2021.01.007
Gempp, L, Benadof. Percepción de apoyo familiar de adultos mayores residentes en establecimientos de larga estadía. Revista Chilena de Salud Pública. 2018; 21(2): 142-149. Disponible en: https://revistasaludpublica.uchile.cl/index.php/RCSP/article/view/48911 DOI: https://doi.org/10.5354/0719-5281.2017.48911
Guerrero RF, Menezes TM, Prado MD, Galindo JA. Espiritualidad y religiosidad para la trascendencia del ser anciano. Rev. Bras. Enferm. 2019; 722: 259-265. Disponible en:http://www.scielo.br/scielo.php?script=sci_arttext&pid=S003471672019000800259&lng=en
Puchalski C. Spirituality in the cancer trajectory. In: Annals of Oncology. Oxford University Press. 2012; 49-55. Available from: https://academic.oup.com/annonc/articlelookup/doi/10.1093/annonc/mds088 [Internet] [citado el 21 de junio de 2021]. DOI: https://doi.org/10.1093/annonc/mds088
Salas C, Taboada P. Espiritualidad en medicina: análisis de la justificación ética en Puchalski. Rev. méd. Chile. 2019; 147(9): 1199-1205. Disponible en: https://scielo.conicyt.cl/scielo.php?script=sci_arttext&pid=S0034-98872019000901199&lng=es [Internet] [citado 2021 Ene 20]. DOI: https://doi.org/10.4067/s0034-98872019000901199
Organización Mundial de la Salud. Plan de acción sobre la salud de las personas mayores incluido el envejecimiento activo y saludable. Washington: OMS/OPS, 2009; 3-5.
Arroyo MC, Vázquez L. Percepción de personas mayores sobre la atención recibida en instituciones de salud de la ciudad de Durango. Revista pueblos y fronteras digital. 2016; 11(21): 144- 172. https://doi.org/10.22201/cimsur.18704115e.2016.21.12 DOI: https://doi.org/10.22201/cimsur.18704115e.2016.21.12
Ruelas MG, Pelcastre BE, Reyes H. Maltrato institucional hacia el adulto mayor: percepciones del prestador de servicios de salud y de los ancianos. Salud pública Méx. 2014; 56(6): 631-637. Disponible en: http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S0036-36342014000600013&lng=es [citado 2021 Jun 17]. DOI: https://doi.org/10.21149/spm.v56i6.7390
Priego-Álvarez HR, Arellano Zuñiga KCC, Avalos García MI, Bracqbien Noygues CS. Invisibilidad del adulto mayor con VIH/SIDA: La percepción del médico de primer nivel en Tabasco, México. 2020; 36(2). Disponible en: https://rcientificas.uninorte.edu.co/index.php/salud/article/view/13004 http://dx.doi.org/10.14482/sun.36.2.616.979 [citado 9 de junio de 2021]. DOI: https://doi.org/10.14482/sun.36.2.616.979
Adams Y. Maltrato en el adulto mayor institucionalizado: Realidad e invisibilidad, Revista Médica Clínica Las Condes. 2012; 23 (1): 84-90. https://doi.org/10.1016/S0716- 8640(12)70277-8. https://www.sciencedirect.com/science/article/pii/S0716864012702778 DOI: https://doi.org/10.1016/S0716-8640(12)70277-8
Wong A, Chau AKC, Fang Y, Woo J. Illuminating the Psychological Experience of Elderly Loneliness from a Societal Perspective: A Qualitative Study of Alienation between Older People and Society. International Journal of Environmental Research and Public Health. 2017; 14(7):824. https://doi.org/10.3390/ijerph14070824 DOI: https://doi.org/10.3390/ijerph14070824
Shepherd B, Brochu P. How do stereotypes harm older adults? A theoretical explanation for the perpetration of elder abuse and its rise, Aggression and Violent Behavior. 2021; (57). https://doi.org/10.1016/j.avb.2020.101435. DOI: https://doi.org/10.1016/j.avb.2020.101435
Rondón LM, Ruiz RR. The impact of positive social relations on the quality of life of older people. An alternative to medicalization from an integral perspective. Chapter 4 Editor(s): Colin R. Martin, Victor R. Preedy, Rajkumar Rajendram, Assessments, Treatments and Modeling in Aging and Neurological Disease, Academic Press. 2021; 29-37. https://doi.org/10.1016/B978-0-12- 818000-6.00004-4 DOI: https://doi.org/10.1016/B978-0-12-818000-6.00004-4
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.