Diffuse external otitis: A trivial pathology?
Keywords:
external otitis, otitis, ear DiseaseAbstract
External otitis is a frequent pathology in the medical consultation, it is estimated that 10% of people will suffer it at least once in their life, the acute presentation compromises the external auditory canal of infectious origin in 90% of cases, called diffuse external otitis (DEO). The objective of this article is to present the best current evidence that allows a general description of the pathology, for which a search of scientific literature was carried out in recognized databases, finding that it was characterized microbiologically by the presence of Pseudomonas aeruginosa and Staphylococcus aureus, clinically, patients refer to otalgia generating a variety of differential diagnoses, and for treatment, a classification must be made based on various variables (age, atrial compromise, and immune status) in order to determine the appropriate therapeutic route.
Metrics
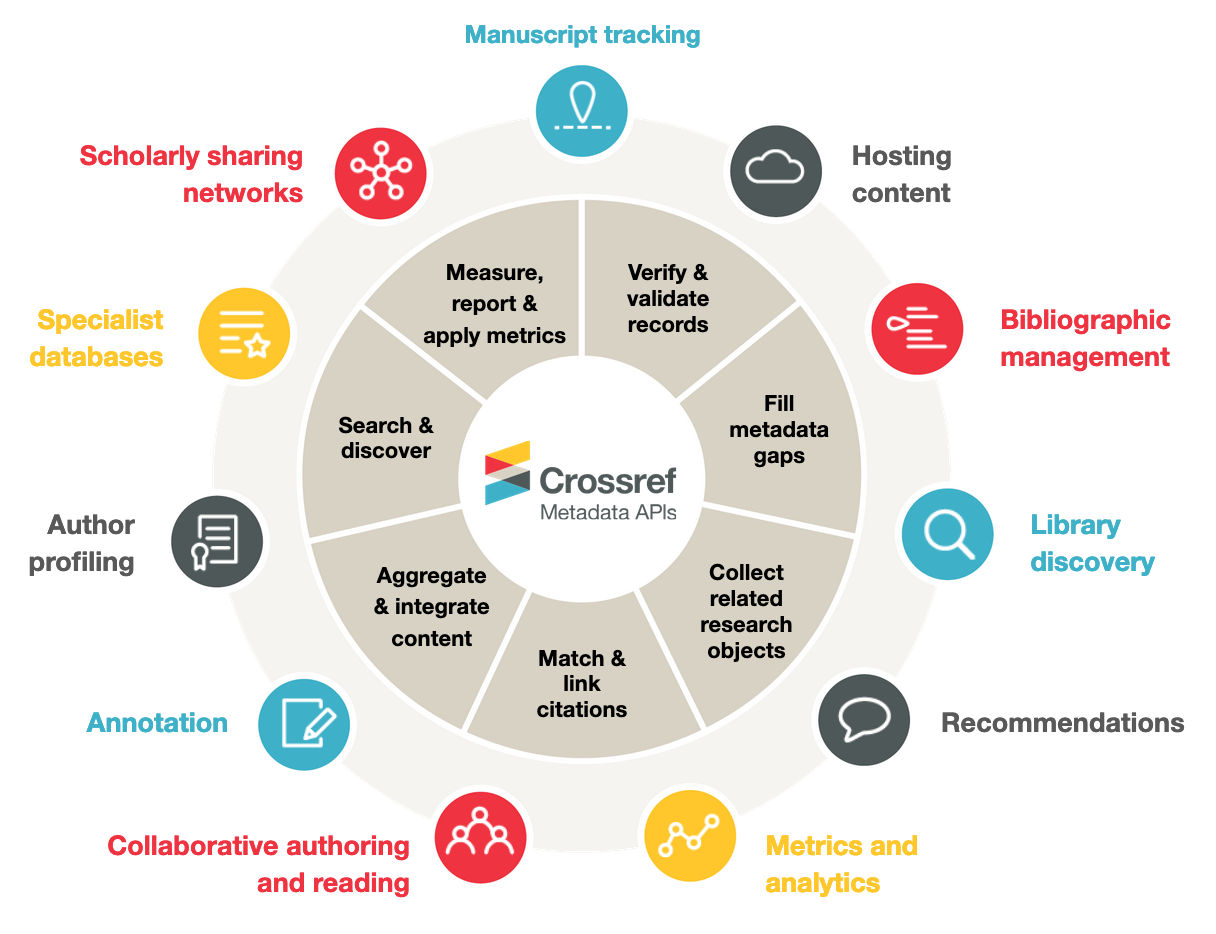
References
Medina-Blasini Y, Sharman T. Otitis Externa [Internet]. StatPearls [Internet]. StatPearls Publishing; 2020 [citado 19 de junio de 2021]. Disponible en: https://www.ncbi.nlm.nih.gov/books/NBK556055/
Wiegand S, Berner R, Schneider A, Lundershausen E, Dietz A. Otitis Externa. Dtsch Arztebl Int. marzo de 2019;116(13):224-34.
Hajioff D, MacKeith S. Otitis externa. BMJ Clin Evid. 15 de junio de 2015;2015:0510.
Wipperman J. Otitis Externa. Primary Care: Clinics in Office Practice. 1 de marzo de 2014;41(1):1-9.
Rosenfeld RM, Schwartz SR, Cannon CR, Roland PS, Simon GR, Kumar KA, et al. Guía de práctica clínica: otitis externa aguda. Otolaryngol Head Neck Surg. 1 de febrero de 2014;150(1_suppl):S1-24.
[External otitis in children: etiology and principes of therapy]. Vestn Otorinolaringol. 2011;(6):113-6.
Larach F, Astorquiza C. OTITIS EXTERNA: DIAGNÓSTICO Y MANEJO PRÁCTICO. Rev Med Clin Condes. 1 de noviembre de 2016;27(6):898-904.
Balcázar Rincon LE, Ramírez Alcántara YL[Internet]. [citado 25 de septiembre de 2021]. Disponible en: https://www.medigraphic.com/pdfs/quirurgicas/rmq-2014/rmq141o.pdf
Spernovasilis N, Psichogiou M, Poulakou G. Skin manifestations of Pseudomonas aeruginosa infections. Current Opinion in Infectious Diseases. abril de 2021;34(2):72-9.
Cervantes-García E, García-González R, Salazar-Schettino PM. Características generales del Staphylococcus aureus. :13.
Sastre MAD, Zannin I, Antolín JJ. PATOLOGÍA INFLAMATORIA DEL OÍDO EXTERNO. OTITIS EXTERNA. OTITIS EXTERNA MALIGNA. :15.
Ghanpur AD. Comparison of Microbiological Flora in the External Auditory Canal of Normal Ear and an Ear with Acute Otitis Externa. JCDR [Internet]. 2017 [citado 19 de junio de 2021]; Disponible en: http://jcdr.net/article_fulltext.asp?issn=0973-709x&year=2017&volume=11&issue=9&page=MC01&issn=0973-709x&id=10556
Schaefer P, Baugh RF. Acute Otitis Externa: An Update. AFP. 1 de diciembre de 2012;86(11):1055-61.
Mittal A, Kumar S. Role of pH of External Auditory Canal in Acute Otitis Externa. Indian J Otolaryngol Head Neck Surg. enero de 2014;66(1):86-91.
Musa TS, Bemu AN, Grema US, Kirfi AM. Pattern of otitis externa in Kaduna Nigeria. Pan Afr Med J [Internet]. 30 de junio de 2015 [citado 19 de junio de 2021];21. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4546771/
Vaduva C, Gómez JIT, Zaid DM, Rivera-Rodríguez T. Patología infecciosa aguda de foco otorrinolaringológico. Medicine (Madr). noviembre de 2019;12(91):5339-51.
Balch G, Heal C, Cervin A, Gunnarsson R. Oral corticosteroids for painful acute otitis externa (swimmer’s ear): A triple-blind randomised controlled trial. Aust J Gen Pract. agosto de 2019;48(8):565-72.
Kaushik V, Malik T, Saeed SR. Interventions for acute otitis externa. Cochrane Database of Systematic Reviews [Internet]. 2010 [citado 21 de junio de 2021];(1). Disponible en: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004740.pub2/full
Mösges R, Nematian-Samani M, Hellmich M, Shah-Hosseini K. A meta-analysis of the efficacy of quinolone containing otics in comparison to antibiotic-steroid combination drugs in the local treatment of otitis externa. Curr Med Res Opin. octubre de 2011;27(10):2053-60.
Published guidance and advice | Guidance | NICE [Internet]. NICE; [citado 22 de junio de 2021]. Disponible en: https://www.nice.org.uk/guidance/published?type=apa&title=antimicrobial
Mughal Z, Swaminathan R, Al-Deerawi HB, Henney S, Bickerton R. A Systematic Review of Antibiotic Prescription for Acute Otitis Externa. Cureus. 13(3):e14149.
M.S SR, Rajkamal M, Bharadwaj B. A COMPARATIVE STUDY BETWEEN MUPIROCIN AND MAGSULPH-GLYCERINE WICK TREATMENT IN THE MANAGEMENT OF ACUTE OTITIS EXTERNA. jebmh. 7 de marzo de 2018;5(11):970-3.
Arés Álvarez F, Martínez de la Ossa Sáenz-López R, Alfayate Miguélez S, Arés Álvarez F, Martínez de la Ossa Sáenz-López R, Alfayate Miguélez S. Quinolonas en Pediatría. Pediatría Atención Primaria. junio de 2017;19(74):e83-92.
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.